AsianScientist (Apr. 03, 2024) – Type 2 diabetes (DM) is a complex metabolic disorder characterized by high blood sugar levels. According to the World Health Organization (WHO), the prevalence of type 2 diabetes has risen dramatically in all countries, irrespective of their income levels, in the past three decades. WHO estimates over 95% of people with diabetes have type 2 diabetes. It used to occur mainly in adults, but now, more children are being diagnosed with it. About 19% of adults worldwide have severe gum diseases, adding up to over 1 billion cases globally.
People with DM often suffer from periodontitis, a serious gum infection that damages the gums and bone supporting the teeth, leading to tooth loss. However, the complex nature of how these two conditions affect each other was not fully understood.
Now, a new study by researchers from Korea offers the first explanation of how periodontitis and diabetes are linked at the overall and cellular levels of the immune system. The study was conducted by researchers from Pusan National University (PNU) in Busan, South Korea, and was published in Clinical and Translational Medicine.
Even though periodontitis is a common condition in people with diabetes, its effects on health and how it interacts with type 2 diabetes were not fully explored. Previous studies only looked at how the immune system reacts in the gums and missed the bigger picture of how there might be affects in the entire body.
To understand the relationship between the two conditions, the scientists collected blood cells from a mixed group comprising 11 healthy people, 10 with gum disease but no diabetes (PD), and six people with both gum disease and diabetes (PDDM).
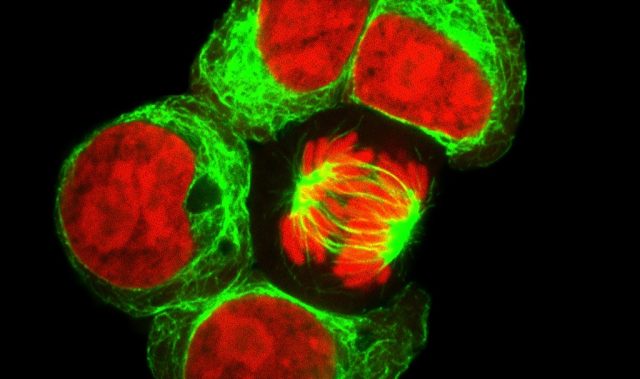
They then analyzed these cells using a cutting-edge single-cell RNA sequencing technique, which helps identify different cell types and their functions within tissues or organisms. The scientists then compared the differences between the groups from an intracellular and intercellular perspective, studying specific types of immune cells in the blood. They found that certain cells became more inflammatory in both the PD and PDDM groups.
RESISTIN, which stands for ‘resistance to insulin,’ is a significant molecule that causes inflammation and is associated with diabetes and other chronic inflammatory conditions. In people with diabetes, there were more cells with RESISTIN. This was true for both gum disease (PD) and diabetes (PDDM) groups. RESISTIN levels in the blood were higher in both PD and PDDM groups than in healthy individuals, suggesting it interacts with the bloodstream.
The study also found that the RESISTIN pathway was more active in both PD and PDDM groups, especially in certain types of white blood cells (essential parts of the immune system) called classical monocytes. This finding is significant as it suggests a common pathway that affects the relationship between gum disease and diabetes. The discovery of RESISTIN in the blood of gum disease patients without other diseases shows its role in inflammation and its potential as a treatment target to lower diabetes risk in these patients.
The results show significant changes in the immune system in patients with both gum disease and diabetes, suggesting that gum disease might precede diabetes. Likewise, the detection of RESISTIN in the blood of patients with gum disease but no other diseases suggest it might be a target for treatment to reduce the risk of diabetes in these patients.
“Our study promises to transform our understanding of the complex interplay between these two prevalent health conditions and sheds light on the systemic impact of these conditions, offering a potential avenue for targeted interventions,” said Yun Hak Kim, assistant professor at the Department of Anatomy at Pusan National University’s (PNU) School of Medicine. He is also the head professor in the Department of Interdisciplinary Science of Genomic Science.
—
Source: Pusan National University; Image: Shutterstock
The paper can be found at: Immunological link between periodontitis and type 2 diabetes deciphered by single-cell RNA analysis
Disclaimer: This article does not necessarily reflect the views of AsianScientist or its staff.