Asian Scientist (May 30, 2022) — Researchers at the University of Tsukuba, Japan, have unraveled the mechanism by which antibiotic resistance is transferred among bacteria. Methicillin-resistant Staphylococcus aureus (MRSA) bacteria is the leading cause of staph infections worldwide. Staph infections range from skin infections, food poisoning, pneumonia to toxic shock syndrome among others. These infections occur when bacteria enter the skin or body through a cut, wound, or contaminated food.
MRSA carries the mobile genetic element SCCmec. Mobile genetic elements are segments of DNA that encode enzymes and other proteins, which mediate the movement of DNA within genomes or between bacterial cells. The SSCmec carries the mecA gene, which is responsible for making Staphylococcus aureus resistant to methicillin and widely used beta-lactam antibiotics like penicillin and cephalosporins.
“Mobile genetic elements carrying antibiotic resistance traits spread horizontally among bacteria” but the method responsible for SCCmec transfer was not known, said Mais Maree, a doctoral student at the University of Tsukuba. She is also the lead author of the study published in Nature Communications.
Staphylococcus aureus is a common bacterium that lives on the skin or in the nose of humans and is generally harmless. However, in certain situations like a weakened immune system or an open wound, it can cause harmful infections. When staphylococci are resistant to treatment with antibiotics, they become especially dangerous. The MRSA strain of Staphylococcus aureus, which is resistant to the antibiotic methicillin, has become a serious problem worldwide.
In the first part of the study, the researchers aimed to clarify the growth conditions in which S. aureus are able to take up genetic material from the environment outside their cell walls and incorporate it into their genome. In the second part, they tested if this natural transformation could mediate the transfer of SCCmec among bacteria.
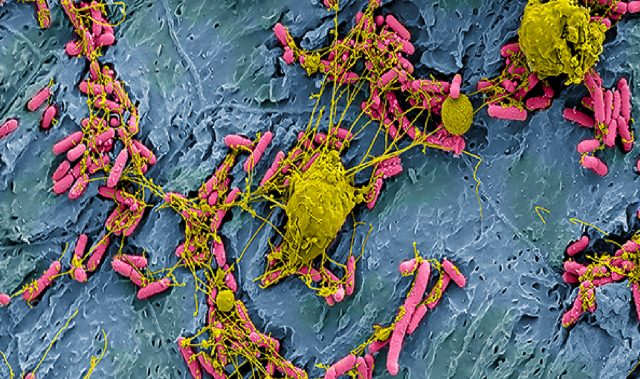
To detect the transfer of antibiotic resistance genes, the researchers grew a high number of bacterial cells in a polystyrene plate, let them settle at the bottom and form a rigid biofilm. Biofilms are complex structures of bacteria sticking to each other and growing on a surface. In this growth condition of biofilms, living bacteria cells were able to uptake DNA having antibiotic resistance marker—SCCmec—from dead bacteria, and incorporate it into its genome.
Then the researchers applied antibiotic to select and detect those cells that had successfully incorporated SCCmec with mecA. The cells that did not uptake this mobile DNA will get killed.
“By using this simple method, we were able to detect the transfer of antibiotic resistance genes through the mechanism of natural transformation,” said Maree.
This study informs how Staphylococcus aureus develop antimicrobial resistance. By interfering with this process, the spread of antimicrobial resistance by SCCmec elements can be contained.
“Targeting biofilm formation could be a promising approach for preventing the evolution of staphylococcal bacteria and the spread of bacterial resistance by the transfer of SCC mobile elements,” said senior author and Professor, Faculty of Medicine, University of Tsukuba.
Next, Maree and her team will further investigate how MRSA emerges and maintains SCCmec under different environmental conditions.
—
Source: University of Tsukuba ; Photo: Unsplash
The article can be found at: Maree et. al (2022) Natural transformation allows transfer of SCCmec-mediated methicillin resistance in Staphylococcus aureus biofilms